The Case Against Sugar
By Gary Taubes, 2016
Introduction: Why Diabetes?
Mary H — an unmarried woman, twenty-six years of age, came to the Out Patient Department of the Massachusetts General Hospital on August 2, 1893. She said her mouth was dry, that she was
drinking water all the timeand was compelled to rise three to four times each night to pass her urine. She feltweak and tired.Her appetite was variable; the bowels constipated and she had a dizzy headache. Belching of gas, a tight feeling in the abdomen, and aburningin the stomach followed her meals. She was Short of breath.
Elliott Joslin was a medical student at Harvard in the summer of 1893, working as a clinical clerk at Massachusetts General Hospital, when he documented his first consultation with a diabetic patient. He was still a good three decades removed from becoming the most influential diabetes specialist of the twentieth century. The patient was Mary Higgins, a young immigrant who had arrived from Ireland five years previously and had been working as a domestic in a Boston suburb. She had a severe form of diabetes mellitus,
Joslin noted, and her kidneys were already succumbing to the strain put upon them
by the disease.
Joslin’s interest in diabetes dated to his undergraduate days at Yale, but it may have been Higgins who catalyzed his obsession. Over the next five years, Joslin and Reginald Fitz, a renowned Harvard pathologist, would comb through the hundreds of volumes
of handwritten case notes of the Massachusetts General Hospital, looking for information that might shed light on the cause of the disease and perhaps suggest how to treat it. Joslin would travel twice to Europe, visiting medical centers in Germany and Austria, to learn from the most influential diabetes experts of the era.
In 1898, the same year Joslin established his private practice to specialize in the treatment of diabetics, he and Fitz presented their analysis of the Mass General case notes at the annual meeting of the American Medical Association in Denver. They had examined the record of every patient treated at the hospital since 1824. What they saw, although they didn’t recognize it at the time, was the beginning of an epidemic.
Among the forty-eight thousand patients treated in that time period, a year shy of three-quarters of a century, a total of 172 had been diagnosed with diabetes. These patients represented only 0.3 percent of all cases at Mass General, but Joslin and Fitz detected a clear trend in the admissions: the number of patients with diabetes and the percentage of patients with diabetes had both been increasing steadily. As many diabetics were admitted to Mass General in the thirteen years after 1885 as in the sixty-one years prior. Joslin and Fitz considered several explanations, but they rejected the possibility that the disease itself was becoming more common. Instead, they attributed the increase in diabetic patients to a wholesome tendency of diabetics to place themselves under careful medical supervision.
It wasn’t that more Bostonians were succumbing to diabetes year to year, they said, but that a greater proportion of those who did were taking themselves off to the hospital for treatment.
By January 1921, when Joslin published an article about his clinical experience with diabetes for The Journal of the American Medical Association, his opinion had changed considerably. He was no longer talking about the wholesome tendencies of diabetics to seek medical help, but was using the word epidemic
to describe what he was witnessing. On the broad street of a certain peaceful New England village there once stood three houses side by side,
he wrote, apparently talking about his hometown of Oxford, Massachusetts. Into these three houses moved in succession four women and three men — heads of families — and of this number all but one subsequently succumbed to diabetes.
Joslin suggested that had these deaths been caused by an infectious disease — scarlet fever, perhaps, or typhoid, or tuberculosis — the local and state health departments would have mobilized investigative teams to establish the vectors of the disease and prevent further spread. Consider the measures,
he wrote, that would have been adopted to discover the source of the outbreak and to prevent a recurrence.
Because diabetes was a chronic disease, not an infectious one, and because the deaths occurred over years and not in the span of a few weeks or months, they passed unnoticed. Even the insurance companies,
Joslin wrote, failed to grasp their significance.
We've grown accustomed, if not inured, to reading about the ongoing epidemic of obesity. Fifty years ago, one in eight American adults was obese; today the number is greater than one in three. The World Health Organization reports that obesity rates have doubled worldwide since 1980; in 2014, more than half a billion adults on the planet were obese, and more than forty million children under the age of five were overweight or obese. Without doubt we’ve been getting fatter, a trend that can be traced back in the United States to the nineteenth century, but the epidemic of diabetes is a more intriguing, more telling phenomenon.
Diabetes was not a new diagnosis at the tail end of the nineteenth century when Joslin did his first accounting, rare as the disease might have been then. As far back as the sixth century B.C., Sushruta, a Hindu physician, had described the characteristic sweet urine of diabetes mellitus, and noted that it was most common in the overweight and the gluttonous. By the first century A.D., the disease may have already been known as diabetes
— a Greek term meaning siphon
or flowing through
— when Aretaeus of Cappodocia described its ultimate course if allowed to proceed untreated: The patient does not survive long when it is completely established, for the marasmus [emaciation] produced is rapid, and death speedy. Life too is odious and painful, the thirst is ungovernable, and the copious potations are more than equaled by the profuse urinary discharge … If he stop for a very brief period, and leave off drinking, the mouth becomes parched, the body dry; the bowels seem on fire, he is wretched and uneasy, and soon dies, tormented with burning thirst.
Through the mid-nineteenth century, diabetes remained a rare affliction, to be discussed in medical texts and journal articles but rarely seen by physicians in their practices. As late as 1797, the British army surgeon John Rollo could publish An Account of Two Cases of the Diabetes Mellitus,
a seminal paper in the history of the disease, and report that he had seen these cases nineteen years apart despite, as Rollo wrote, spending the intervening years observ[ing] an extensive range of disease in America, the West Indies, and in England.
If the mortality records from Philadelphia in the early nineteenth century are any indication, the city’s residents were as likely to die from diabetes, or at least to have diabetes attributed as the cause of their death, as they were to be murdered or to die from anthrax, hysteria, starvation, or lethargy.
At Massachusetts General Hospital, the very same handwritten medical records that Joslin would later analyze reveal that for twenty of the forty-five years between 1824 and 1869 there was not a single case of diabetes. In none of these years were there more than three cases.
In 1890, Robert Saundby, a former president of the Edinburgh Royal Medical Society, presented a series of lectures on diabetes to the Royal College of Physicians in London in which he estimated that less than one in every fifty thousand died from the disease. Diabetes, said Saundby, is one of those rarer diseases
that can only be studied by physicians who live in great cent[er]s of population and have the extensive practice of a large hospital from which to draw their cases.
Saundby did note, though, that the mortality rate from diabetes was rising throughout England, in Paris, and even in New York. (At the same time, one Los Angeles physician, according to Saundby, reported in seven years’ practice he had not met with a single case.
) The truth,
Saundby said, is that diabetes is getting to be a common disease in certain classes, especially the wealthier commercial classes.
William Osler, the legendary Canadian physician often described as the father of modern medicine,
also documented both the rarity and the rising tide of diabetes in the numerous editions of his seminal textbook, The Principles and Practice of Medicine. Osler joined the staff at Johns Hopkins Hospital in Baltimore when the institution opened in 1889. In the first edition of his textbook, published three years later, Osler reported that, of the thirty-five thousand patients under treatment at the hospital since its inception, only ten had been diagnosed with diabetes. In the next eight years, 156 cases were diagnosed. Mortality statistics, wrote Osler, suggested an exponential increase in those reportedly dying from the disease — nearly doubling between 1870 and 1890 and then more than doubling again by 1900.
By the late 1920s, Joslin’s epidemic of diabetes had become the subject of newspaper and magazine articles, while researchers in the United States and Europe were working to quantify accurately the prevalence of the disease, in a way that might allow meaningful comparisons to be drawn from year to year and decade to decade. In Copenhagen, for instance, the number of diabetics treated in the city’s hospitals increased from ten in 1890 to 608 in 1924 — a sixty-fold increase. When the New York City health commissioner Haven Emerson and his colleague Louise Larimore published an analysis of diabetes mortality statistics in 1924, they reported a 400 percent increase in some American cities since 1900 — almost 1,500 percent since the Civil War.
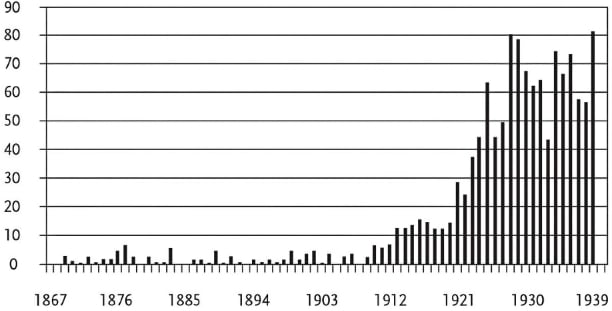
Diabetes admissions, Pennsylvania Hospital, Philadelphia
Despite all this, the disease remained a relatively rare one. When Joslin, working with Louis Dublin and Herbert Marks, both statisticians with the Metropolitan Life Insurance Company, examined the existing evidence in 1934, he again concluded that diabetes was rapidly becoming a common disease, but only by the standards of the day. He conservatively estimated — based on what he considered careful studies done in New York, Massachusetts, and elsewhere — that only two to three Americans in every thousand had diabetes.
Times have certainly changed. In 2012, the latest year for which the Centers for Disease Control (CDC) have provided estimates, one in every seven to eight adults in this country had diabetes — 12 to 14 percent, depending on the criteria used to diagnose it. Another 30 percent are predicted to get diabetes at some point during their lives. Almost two million Americans were diagnosed with diabetes in 2012 — one case every fifteen to sixteen seconds. Among U.S. military veterans, one in every four patients admitted to VA hospitals suffers from diabetes.
The great proportion of this tidal wave of diabetics — perhaps 95 percent — have what is now known as type 2 diabetes, the form of the disease, as Sushruta would have said over two thousand years ago, that associates with overweight and obesity. A small proportion have type 1, typically children. This is the acute form of the disease, and it kills, if untreated, far more quickly. Because type 2 diabetes is so much more common, when I refer to diabetes in this book I will be referring to the type 2 form or both type 2 and type 1 together, unless specified otherwise. Both type 1 and type 2 diabetes have been increasing in prevalence for the past 150 years; in both, the increase has been dramatic.
Those afflicted with diabetes will die at greatly increased rates from heart disease or stroke, from kidney disease — the disease is now considered the cause of more than 40 percent of cases of kidney failure — and diabetic coma. Without appropriate treatment (and occasionally even with), their eyesight will deteriorate (often a first symptom); they’ll suffer nerve damage; their teeth will decay and fall out; they’ll get foot ulcers and gangrene; and they'll lose limbs to amputation. Six in every ten lower-limb amputations in adults are due to diabetes — some seventy-three thousand of them in 2010 alone. A dozen classes of drugs are now available to treat the disease, and the market for diabetic drugs and devices in the United States alone is over thirty billion dollars yearly. Drugstore chains now offer free tests to customers to check levels of blood sugar, hoping to sell home-testing kits to those whose blood sugar might happen to show up borderline or high.
The obvious questions are: Why have things changed so? How did we get here? What forces of nature or environment or lifestyle have led to diabetes in one out of every eleven Americans, children and adults together?
One way to avoid answering this question is to assume that historical trends in diabetes prevalence constitute unreliable evidence. Who knows what was really going on fifty or a hundred years ago? And, indeed, it’s surprisingly difficult to quantify with any confidence the changing prevalence of a chronic disease in a population. Such issues as the criteria by which it’s diagnosed, how much attention physicians, the public, and the media pay to it, the availability of treatment and how well those treatments work, the longevity of the population, and whether the disease is more common with age will all confound any authoritative attempts to establish reliably how the actual occurrence of a chronic disease has changed with time. It's a very good bet, though, that had one in eleven Americans been afflicted with diabetes in the nineteenth century, the hospital inpatient records of those eras would have looked dramatically different, as would the number of deaths attributed to diabetes. As Saundby wrote in 1901, Diabetes is in all cases a grave disease … Life seems to hang by a thread, a thread often cut by a very trifling accident.
For the past century, the observation that diabetes is increasing in the population — transitioning from a rare disease to a common one and now to a scourge — has remained a constant theme in the medical literature. In 1940, Russell Wilder, the leading diabetologist at the Mayo Clinic, reported that diabetes admissions had been increasing steadily at the clinic for the previous twenty years. The incidence of diabetic morbidity is unknown,
he wrote, but the indications that it is increasing are very clear.
Ten years later, Joslin himself referred to the appalling increase in diabetes,
which he now considered an inescapable fact of life. In 1978, Kelly West, the leading American authority on diabetes epidemiology — the study of how diseases move through populations — suggested that diabetes had already killed more people in the twentieth century than all wars combined. Diabetes mellitus has become one of the most important of human problems,
he wrote, calling it a significant cause of disease and death in all countries and all major races.
Epidemic increases in the occurrence of diabetes, as West suggested, were not a localized phenomenon. Diabetes was virtually unknown or at least undiagnosed in China, for instance, at the turn of the twentieth century. One British physician reported seeing only one case of the disease among twenty-four thousand outpatients in Nanking, although all drawn from the lower classes of society.
Another reported only two cases among the twelve thousand inpatients treated in his hospital. In the 1980s, the prevalence of diabetes in the Chinese population at large was still estimated to be approximately 1 percent. The latest estimates are that 11.6 percent of the adult population is diabetic — one in nine, more than 110 million Chinese in total. Almost half a billion Chinese are believed to be pre-diabetic.
The prevalence of both diabetes and pre-diabetes was considered vanishingly small among Inuit in Greenland, Canada, and Alaska through the 1960s — Eight Alaskan Eskimos are now known to have diabetes,
reported one article in the Journal of the American Medical Association in 1967. By the 1970s, diabetes was still rare, but researchers were now documenting the increasing appearance of a pre-diabetic condition, glucose intolerance. In recent studies, diabetes rates in the Inuit are now at 9 percent — one in every eleven individuals — similar to the levels in Canada and the United States as a whole.
The same epidemic patterns have been observed in Native American tribes (particularly the Pima population in Arizona, as we'll discuss later) and in the First Nations People of Canada. In many of these populations, one out of every two adults now has diabetes. In some cases — the Ojibwa Cree people of Sandy Lake in northern Ontario, for instance — diabetes, if it existed, was undiagnosed in the population as late as the 1960s. In 1974, when Kelly West examined the available data on diabetes in Native American populations, he concluded that the disease had been rare to nonexistent prior to the 1940s — both civilian and military physicians had carried out health surveys — and yet, by the mid-1960s, research, including his own, was documenting previously unafflicted populations in which one in four adults was diabetic. (When researchers charted the number of cases diagnosed each year in the Navajo from the 1950s through the 1980s, the resulting graph looked almost identical to that on this page from Pennsylvania Hospital in Philadelphia a century earlier.)
Similar patterns have been observed in Polynesians, Micronesians, and Melanesians in the South Pacific; in aboriginal populations in Australia; in Maoris in New Zealand; and in populations throughout the Middle East, Asia, and Africa. In fact, anywhere populations begin eating Western diets and living Western lifestyles — whenever and wherever they’re acculturated or urbanized, as West noted in 1978 — diabetes epidemics follow.
So what happened? Whats happening? Something changed dramatically in our diets, our lifestyle, or our environment to trigger these unprecedented epidemics of diabetes; but what? As Joslin observed under similar circumstances at a far earlier stage in this epidemic, had this been an infectious disease, the relevant boards of health, the insurance agencies, the newspapers, the country as a whole, would be demanding answers. The CDC and the World Health Organization would have established panels of expert investigators to pry into every crevice of our assumptions about the cause of this disease to see where we might have misunderstood its etiology. Such is not the case.
Prior to the 1970s, public-health authorities and clinicians commenting on the rising tide of diabetes in the populations they studied frequently suggested what to them seemed like the prime suspect — sugar consumption. Here was a disease of carbohydrate metabolism that was becoming increasingly common as populations began consuming sugar — a kind of carbohydrate — at levels that were virtually unimaginable a century before; in some cases, just twenty or thirty years before.
As sugar consumption exploded in the United States and the United Kingdom with the industrial revolution; with the birth of the confectionary, cereal, and soft-drink industries; and with the increasing availability of chocolate bars and ice-cream treats, so did diabetes begin its inexorable climb. When sugar and sugar-rich products spread around the globe, so did diabetes. When peasant farmers throughout Africa, India, Asia, and Central and South
America migrated to towns and cities to become wage earners, and changed their dietary habits accordingly — no longer eating locally grown cereals, starches, and fruits, but instead buying sugary drinks and sugar-laden treats in shops and markets — diabetes made its inevitable appearance. As Kelly West said about the emerging epidemics of diabetes in Native American populations in 1974, Some had been nomadic hunters and meat eaters … while others had derived a substantial majority of their calories from fats … Sugar consumption has been increasing in most, if not all, of the United States tribes in whom diabetes rates have recently increased precipitously. This same association has been observed in Eskimos of Alaska, Canada, and Greenland as well as in Polynesians.
And on those very rare occasions when sugar consumption declined — as it did, for instance, during World War I, because of government rationing and sugar shortages — diabetes mortality invariably declined with it. Rises and falls in sugar consumption,
wrote Haven Emerson and Louise Larimore in 1924, are followed with fair regularity … by similar rises and falls in the death rates from diabetes.
In 1974, when the sugar industry hired pollsters to survey physicians for their attitudes toward sugar, most of those physicians said they thought sugar consumption accelerated the onset of diabetes. (One advertising executive, later asked if his children ate a particularly sugar-rich cereal for which he had modeled the ad Campaign on Snoopy and the Red Baron, admitted that they never did: You need an insulin shot if you eat a bowl of that,
he said.) In 1973, Jean Mayer of the Harvard School of Public Health, probably the most influential nutritionist of the era, was suggesting that sugar plays an etiological role in those individuals who are genetically susceptible to the disease.
Such a statement, of course, raises the obvious question of whether anyone ever gets the disease who isn't genetically susceptible (with the rare exceptions of those individuals who sustain injuries or tumors that affect pancreatic function). Nonetheless, at scientific meetings on sugar and other sweeteners, researchers and clinicians would debate whether or not sugar caused diabetes or only helped it along in those somehow predisposed.
By the late 1970s, though, sugar had mostly vanished from the discussion. Dietary fat had been implicated as a cause of heart disease. Nutritionists and public-health authorities responded by rejecting the idea that sugar could be responsible for the diseases that associated with heart disease, which included both obesity and diabetes.
Researchers had also come to embrace a pair of related assumptions that were poorly tested and might or might not be true. The first is that type 2 diabetes is caused by obesity, because the two diseases are so closely associated, both in populations and in individuals, and obesity typically appears first (although more than one in every ten individuals diagnosed with type 2 diabetes is neither obese nor overweight). The second assumption, as the World Health Organization puts it, is: The fundamental cause of obesity and overweight is an energy imbalance between calories consumed and calories expended.
The only trouble with the American diet,
as Fred Stare, the founder and head of the nutrition department at Harvard University, said in 1976 on national television, is that we eat too damn much.
The overeating was accompanied by a decrease in physical activity, attributed to changing modes of transportation and the mechanization of labor.
Public-health authorities have considered no investigations necessary to explain the obesity and diabetes epidemics, because they have assumed that the cause is obvious. Attempts to prevent diabetes in the United States, Europe, and Asia, and among populations worldwide, are almost invariably aimed at getting these populations to eat smaller portions and fewer calories, perhaps to avoid fatty foods,
as particularly dense sources of calories, and to increase their physical activity.
Meanwhile, the latest surge in this epidemic of diabetes in the United States — an 800 percent increase from 1960 to the present day, according to the Centers for Disease Control — coincides with a significant rise in the consumption of sugar. Or, rather, it coincides with a surge in the consumption of sugars, or what the FDA calls caloric sweeteners
— sucrose, from sugarcane or beets, and high-fructose corn syrup, HFCS, a relatively new invention.
After ignoring or downplaying the role of sugars and sweets for a quarter-century, many authorities now argue that these are, indeed, a major cause of obesity and diabetes and that they should be taxed heavily or regulated. The authorities still do so, however, not because they believe sugar causes disease but, rather, because they believe sugar represents empty calories
that we eat in excess because they taste so good. By this logic, since refined sugar and high-fructose corn syrup don’t contain any protein, vitamins, minerals, antioxidants, or fiber, they either displace other, more nutritious elements of our diet, or simply add extra, unneeded calories to make us fatter. The Department of Agriculture, for instance (in its recent Dietary Guidelines for Americans
), the World Health Organization, and the American Heart Association, among other organizations, advise a reduction in sugar consumption for these reasons primarily.
The empty-calories argument is particularly convenient for the food industry, which would understandably prefer not to see a key constituent of its products — all too often, the key constituent — damned as toxic. The sugar industry played a key role in the general exoneration of sugar that took place in the 1970s, as lIl explain later. Health organizations, including the American Diabetes Association and the American Heart Association, have also found the argument convenient, having spent the last fifty years blaming dietary fat for our ills while letting sugar off the hook.
The empty-calories logic allows companies that sell sugar-rich products, or products in which all the calories come from these sugars, to claim that they, too, are fighting the good fight. They can profess and perhaps believe that they are fighting the scourge of childhood obesity and diabetes — that they are part of the solution, not the problem — by working to educate children on how to eat less, be satisfied with smaller portions, and exercise more, just as Coca-Cola, PepsiCo, Mars, Nestlé, Hershey’s, and a few dozen other companies did in 2009 when they joined up with the Grocery Manufacturers Association, the American Dietetic Association (now the Academy of Nutrition and Dietetics), and the Girl Scouts of the USA to found the Healthy Weight Commitment Foundation. Embracing the notion of empty calories is politically expedient as well. Any politician running for public office is unlikely to benefit from alienating major constituents of the food industry, particularly companies with powerful lobbies, such as the sugar and beverage industries. This is not about demonizing any industry,
as Michelle Obama said in 2010 about Let's Move,
her much-publicized program to combat childhood obesity.
This book makes a different argument: that sugars like sucrose and high-fructose corn syrup are fundamental causes of diabetes and obesity, using the same simple concept of causality that we employ when we say smoking cigarettes causes lung cancer. It’s not because we eat too much of these sugars — although that is implied merely by the terms overconsumption
and overeating
— but because they have unique physiological, metabolic, and endocrinological (i.e., hormonal) effects in the human body that directly trigger these disorders. This argument is championed most prominently by the University of California, San Francisco, pediatric endocrinologist Robert Lustig. These sugars are not short-term toxins that operate over days and weeks, by this logic, but ones that do their damage over years and decades, and perhaps even from generation to generation. In other words, mothers will pass the problem down to their children, not through how and what they feed them (although that plays a role), but through what they eat themselves and how that changes the environment in the womb in which the children develop.
Individuals who get diabetes — the ones in any population who are apparently susceptible, who are genetically predisposed — would never have been stricken if they (and maybe their mothers and their mothers’ mothers) lived in a world without sugar, or at least in a world with a lot less of it than the one in which we have lived for the past 100 to 150 years. These sugars are what an evolutionary biologist might call the environmental or dietary trigger of the disease: the requisite ingredient that triggers the genetic predisposition and turns an otherwise healthy diet into a harmful one. Add such sugars in sufficient quantity to the diet of any population, no matter what proportion of plants to animals they eat — as Kelly West suggested in 1974 about Native American populations — and the result eventually is an epidemic of diabetes, and obesity as well. If this is true, then to make headway against these disorders — to prevent future cases of obesity and diabetes from manifesting themselves, and to reverse the epidemics that are now ongoing — we must show these sugars and the businesses that sell them for what they truly are.
The implications of the case against sugar go far beyond diabetes. Those who are obese or diabetic are also more likely to have fatty liver disease, and this, too, is now epidemic in Westernized populations. The National Institutes of Health estimate that as many as one in four Americans now have the disease, unrelated to alcohol consumption. If untreated, it can progress to cirrhosis of the liver and eventually the need for a liver transplant. Those who are obese and diabetic also tend to be hypertensive; they have a higher risk of heart disease, cancer, and stroke, and possibly dementia and even Alzheimer’s disease as well.
These chronic diseases — the diseases that ultimately kill us in modern Western societies — tend to cluster together in both populations and individual patients. Diabetes, heart disease, cancer, stroke, and Alzheimer’s account for five of the top ten causes of death in the U.S. A conservative estimate is that they cost the medical system and our society, in lost work and productivity, one trillion dollars a year.
Together they’re often referred to as diseases of Western lifestyles, or diseases of Westernization. This cluster has led cancer researchers to suggest that obesity is a cause of cancer. It has led some Alzheimer’s researchers to refer to Alzheimer’s as type 3 diabetes.
All of these diseases have now been linked to a condition known as insulin resistance,
a phenomenon we will examine in depth. Insulin resistance is the fundamental defect present in type 2 diabetes and perhaps obesity as well. So it’s a reasonable possibility that the same thing that causes one of these diseases — type 2 diabetes in particular — causes all of them. It’s what scientists would call the null hypothesis, a starting point for research, discussion, and studies. If sugar and high-fructose corn syrup are the cause of obesity, diabetes, and insulin resistance, then they're also the most likely dietary trigger of these other diseases. Put simply: without these sugars in our diets, the cluster of related illnesses would be far less common than it is today; likewise other disorders that associate with these illnesses, among them polycystic ovary syndrome (PCOS), rheumatoid arthritis, gout, varicose veins, asthma, and inflammatory bowel disease.
If this were a criminal investigation, the detectives assigned to the case would start from the assumption that there was one prime suspect, one likely perpetrator, because the crimes (all the aforementioned diseases) are so closely related. They would only embrace the possibility that there were multiple perpetrators when the single-suspect hypothesis was proved insufficient to explain all the evidence. Scientists know this essential concept as Occam’s Razor. When Isaac Newton said, We are to admit no more causes of natural things than such as are both true and sufficient to explain their appearances,
he was saying the same thing that Albert Einstein, three centuries later, said (or was paraphrased as saying): Everything should be made as simple as possible, but no simpler.
We should begin with the simplest possible hypothesis, and only if that can’t explain what we observe should we consider more complicated explanations — in this case, multiple causes.
This is not, however, how medical researchers and public-health authorities have come to think about these disorders. Despite their faith in the notion that obesity causes or accelerates diabetes and that therefore (in what I will argue is a mistaken assumption) both are diseases of overconsumption and sedentary behavior, they will also defend their failure to curb the ongoing epidemics of these diseases on the basis that these are multifactorial, complex disorders
or multidimensional diseases.
By this they mean that so many factors are involved in the genesis and progression of these diseases — including genetics for sure, epigenetics (the modification of how genes are turned on and off in cells), how much we eat and exercise, perhaps how well we sleep, toxins in the environment, pharmaceuticals, possibly viruses, the effect of antibiotic use on the bacteria in our guts (dysbiosis, as it's now commonly called, or microbial imbalance) — that to identify one ultimate trigger, or one critical component of our modern diets, is to be naive.
The counterargument is simple: Lung cancer is also assuredly a multifactorial, complex disease. Most smokers will never get lung cancer, and at least a tenth of all cases of lung cancer are unrelated to smoking cigarettes, and yet it’s widely accepted — for very good reasons — that smoking is the primary cause. Whether or not obesity and diabetes and their associated diseases are multifactorial, complex disorders, something has to explain their connection with modern Western diets and lifestyles and the epidemics that are both ongoing and almost ubiquitous worldwide. What is it? We are clearly doing something different from what we did fifty years ago, or 150 years ago, and our bodies and health reflect it. Why?
The goal of this book is to clarify the arguments against sugar, correct some of the misconceptions and preconceptions that have dogged the debate for the hundreds of years during which it’s been Ongoing, and provide the perspective and context needed to make reasonable decisions on sugar as individuals and as a society. People are dying today, literally every second, from diseases that seemed virtually nonexistent in populations that didn’t eat modern Western diets or live modern Western lifestyles. Something is killing them prematurely. This book will document the case against sugar as the prime culprit.
In my two previous books on health and nutrition, I discussed the evidence implicating all highly processed and easily digestible carbohydrates in general — grains and starchy vegetables — as well as sugar and high-fructose corn syrup. I suggested that there was something unique about those sugars that then made the other carbohydrate-rich foods a problem as well. So the treatment of the conditions they caused — particularly obesity and diabetes — often required restricting some or all of these carbohydrates, not just sugar.
In this book, the focus is specifically on the role of sugar in our diet, and the likely possibility that the difference between a healthy diet and one that causes obesity, diabetes, heart disease, cancer, and other associated diseases begins with the sugar content. If this is true, it implies that populations or individuals can be at the very least reasonably healthy living on carbohydrate-rich diets, even grain-rich diets, as long as they consume relatively little sugar. As sugar consumption rises and people ingest it over decades, and across generations, it causes insulin resistance and triggers the progression to obesity, diabetes, and the diseases that associate with them. Once this process starts, easily digestible, carbohydrate-rich foods aid and abet it. If the argument is correct, the first necessary step in preventing or avoiding these diseases is to remove the sugars from our diets.
This argument also serves to censure the last century of advice on obesity, diabetes, and nutrition, notwithstanding the best intentions of those who gave it. Despite a century’s worth of evidence implicating sugar as the cause of insulin resistance and diabetes and many, perhaps all, of the diseases that associate with them, the researchers working in these fields, and the health organizations funding this research, chose to ignore it or reject it. Invariably, they did so on the basis of ill-founded assumptions and preconceptions about what other factors might be responsible — dietary fat, or the simplistic idea that eating too many calories of any kind makes us fat. Here I'll be discussing the science as much as the errors in judgment that were made during this time. It’s one thing to claim that sugar is uniquely toxic — perhaps having prematurely killed more people than cigarettes or all wars combined,
as Kelly West said about diabetes itself — but to do so convincingly we have to understand why this conclusion has not been common wisdom.
In the process, I'll be looking at the key scientific issues with a decidedly historical perspective. History is critical to understanding science and how it progresses. In many scientific disciplines — physics, for example — the science is taught with the history attached. Students learn not only what is believed to be true and which conjectures have fallen by the wayside, but on the basis of what experiments and what evidence, and by whose authority and ingenuity. The names of the physicists responsible for the advances in understanding — Newton, Einstein, Maxwell (for his equations of electromagnetism); Heisenberg, Planck, and Schrödinger, among others, for their work in understanding the quantum nature of the universe; and many more — are as well known as many historical figures in politics and other fields. Medicine today, though, as with related fields such as nutrition, is taught mostly untethered from its history. Students are taught what to believe but not always the evidence on which these beliefs are based, and so oftentimes the beliefs cannot be questioned. And medical students are not taught, as physics students typically are, to question everything that has not demonstrably survived the trial-by-fire process of rigorous, methodical testing. Students of any science need to know why they are being asked to believe a particular idea, or why not, and on what grounds. Without the history of the idea, there’s no way to tell and, by implication, no reason to ask.
This is why authorities on diabetes today will often argue that sugar does not cause diabetes but will do so based on little or no awareness of how that conclusion was ultimately reached and on what evidence. It’s why the provenance of the idea that we get fat because we consume more calories than we expend is little known, even by those physicians and researchers who have been (or still are) its die-hard proponents. It’s why the existence of a competing hypothesis of obesity as a hormonal disorder is little known, let alone that this hypothesis is capable of explaining the data and the observations in a way that the energy balance
notion is incapable of doing.
In writing this book, I hope to continue to restore this history to the discussion of how our diets influence our weight and health, and to do so in the context of the vitally important question of sugar in the diet.
I want to clarify a few final points before we continue.
First, I’m going to concede in advance a key point that those who defend the role of sugar in our diet will invariably make. The sugar industry and purveyors of sugar-rich products are right when they say that it cannot be established definitively, with the science as it now stands, that sugar is uniquely harmful — a toxin that does its damage over decades. The evidence is not as clear with sugar as it is with tobacco. This isn't a failure of science but, rather, an issue of its limits.
With tobacco, researchers could compare smokers with nonsmokers and look for the difference in incidence of a single disease — lung cancer — that in nonsmokers, at least, is very rare. These studies were first done in the late 1940s, and the difference observed in these comparisons was so dramatic — heavy smokers had twenty to thirty times the risk of those who had never smoked — that it was effectively impossible to imagine any reasonable explanation other than cigarettes (not that the tobacco industry didn’t try).
With sugar, the best researchers can do is compare individuals all of whom have consumed tremendous amounts of sugar, at least compared with the levels of consumption in non-industrialized societies. If they compare sugar consumers with those who abstain, they're looking at individuals who have vastly different philosophies about how to lead a healthy life and so will differ in many meaningful ways other than just how much sugar they consume. They’re also looking at differences in rates of what are now all-too-common diseases, although whether the diseases would be common in a world without sugar is the question. The study of sugar consumers versus non-consumers entails issues and challenges that simply didn’t exist in the study of cigarettes and lung cancer.
One way to tackle this problem is to compare populations that had no access to sugar, or very little, with those that had plenty — often the same populations twenty, fifty, or a hundred years later. Still, the difference in sugar consumption is just one of the many differences that might explain the differences in health status. It’s possible to assemble a compelling argument with this method (just as a good prosecutor can create a compelling case from circumstantial evidence), but that is not sufficient to establish definitively what is causing the health effects we’re seeing.
Whether we can assemble the kind of evidence that would stand up in a court of law and allow governments to regulate sugar, as they already do tobacco and alcohol, remains to be seen. But whether we have enough evidence and reasonable assumptions to convince ourselves to avoid sugar, to minimize its consumption, and to convince our children to do the same is a different question. That’s the question this book will try to answer.
Second, I need to clarify what exactly we're talking about when we talk about sugar or sugars. This may seem obvious, but it certainly hasn’t been in the past. The controversy over the health effects of sugar — proceeding, as it has, for hundreds of years — is littered with erroneous statements and conclusions that have driven thinking to the current day. Often, if not largely, it is because the individuals considered authorities on the subject often had no true understanding of what they were talking about, and thus no understanding of how different types of sugars — all carbohydrates — might have profoundly different effects on human health. This confusion still exists and still haunts some of the most influential reporting on diet and health, despite the multitudes of articles written on sugar and health in the past decade.
Biochemically, the term sugar
refers to a group of carbohydrate molecules consisting, as the word carbohydrate
implies, of atoms of carbon, hydrogen, and oxygen. The names of these carbohydrates all end in -ose
— glucose, galactose, dextrose, fructose, lactose, sucrose, etc. All of these sugars will dissolve in water, and they all taste sweet to us, although to a greater or lesser extent. When physicians or researchers refer to blood sugar,
they’re talking about glucose, because it constitutes virtually all of the sugar circulating in our blood.
The more common usage of sugar
refers to sucrose, the white crystalline variety that we put in our coffee or tea or sprinkle on our morning cereal. Sucrose in turn is composed of equal parts glucose and fructose, the two smaller sugars (monosaccharides, in the chemical lingo) bonded together to make the larger one (a disaccharide). Fructose, found naturally in fruits and honey, is the sweetest of all these sugars, and it’s the fructose that makes sucrose particularly sweet. Lately, researchers have been asking whether fructose is toxic, because it’s the significant amount of fructose in sugar (sucrose) that differentiates it from other carbohydrate-rich foods, such as bread or potatoes, which break down upon digestion to mostly glucose alone. Because we never consume the fructose without the glucose, though, the appropriate question is whether sucrose, the combination of roughly equal parts fructose and glucose, is toxic, not one alone.
This would be confusing enough without the introduction in the 1970s of high-fructose corn syrup (HFCS), which replaced a significant part of the refined sugar (i.e., sucrose) consumed in the United States over the decade that followed. High-fructose corn syrup comes in different formulations; the most common one is known as HFCS-55, because it’s 55 percent fructose and 45 percent glucose. This ratio was called into question in a 2010 analysis claiming that fructose content in some popular sugary beverages was then as high as 65 percent. In sucrose, the ratio is 50-50. It was created, in fact, to replace sucrose inexpensively when used as the sweetener in soft drinks — specifically Coca-Cola — without any noticeable difference in taste or sweetness.
The U.S. Department of Agriculture includes both sucrose and HFCS in the category of caloric
or nutritive
sweeteners, along with honey and maple syrup — both glucose-fructose combinations — differentiating them from artificial sweeteners such as saccharin, aspartame, and sucralose, which are effectively calorie-free. Public-health authorities often refer to sucrose and HFCS as added sugars
to differentiate them from the component sugars that can be found naturally (in relatively small proportions) in fruits and vegetables.
Because the introduction of HFCS-55 roughly coincided with the beginning of the obesity epidemic in the United States, researchers and journalists later suggested that HFCS was the cause, implying that it was somehow distinct from sugar itself. HFCS was promptly demonized as a particularly pernicious aspect of the diet — ‘the flashpoint for everybody’s distrust of processed foods,
as the New York University nutritionist Marion Nestle has described it — and that’s often still considered to be the case. This is why cans of Pepsi sweetened by sucrose rather than high-fructose corn syrup proudly proclaim that they contain natural sugar.
Newman’s Own lemonade, sweetened with sucrose (cane sugar,
as the label says), proclaims prominently on the carton that it contains no high fructose corn syrup.
In 2010, the Corn Refiners Association petitioned the Food and Drug Administration to allow it to refer to high-fructose corn syrup as corn sugar
on food labels, thus trying to avoid this demonization process. The sugar industry promptly sued them to prevent it from happening, at which point the Corn Refiners countersued. In 2012, the FDA denied the Corn Refiners’ petition — sugar, the FDA said, is a solid, dried, and crystallized sweetener
and HFCS is not — and so the latter is still clearly identifiable as both syrupy and derived from corn.
All of this controversy, however, though it may benefit the sugar (sucrose) industry in particular, serves only to obfuscate the key point: high-fructose corn syrup is not fructose, any more than sucrose is. (The reason for the appellation high fructose
is that HFCS has a greater proportion of fructose to glucose than previous corn syrups, which date back to the nineteenth century and were never sweet enough to challenge the primacy of sucrose in foods and beverages.) Our bodies appear to respond the same way to both sucrose and HFCS. In a 2010 review of the relevant science, Luc Tappy, a researcher at the University of Lausanne in Switzerland, who is considered by biochemists who study fructose to be among the world’s foremost authorities on the subject, said there was not the single hint
that HFCS was more deleterious than other sources of sugar. The question I'll be addressing in this book is whether they are both benign, or both harmful — not whether one is worse than the other.
My usage of the words sugar
or sugars
throughout the text will depend on context. If I’m speaking about the present, when sucrose and high-fructose corn syrup are used to an equal extent, lIl use sugar
to refer to both. If the context is prior to the introduction of high-fructose corn syrup in the late 1970s, then sugar
will only mean sucrose, and I'll often qualify it by describing it as either beet sugar or cane sugar. If I’m referring to specific (monosaccharide) sugars — fructose, glucose, lactose, etc. — then that, too, will be clear from the context.
The last issue that requires clarification before we continue is that of how much of these sugars (i.e., caloric sweeteners) we actually consume or, for that matter, ever did. Through the 1970s, the per capita consumption numbers cited by government organizations, historians, and journalists — the numbers I typically use in this book — would have been for sugar deliveries,
as the Department of Agriculture now refers to them. This is the amount that industry makes available for consumer use. The formula is simple: domestic production plus imports minus exports, all divided by the current population. Governments acquire these numbers for tax, tariff, and other purposes, and they do it reasonably well. Hence, these numbers are (relatively) reliable, as are trends based on these numbers. We can assume, for instance, that when the USDA reports that 114 pounds of sugar and HFCS were delivered to retailers in 2014, that number can be meaningfully compared with the 153 pounds delivered in 1999, when deliveries (and, so we assume, consumption) peaked in the United States, and both can be compared with the few tens of pounds delivered per capita two hundred years ago.
Beginning in the 1980s, however, with a Food and Drug Administration report that we will discuss in chapter 8, authorities have often tried to estimate how much of this available sugar is actually consumed. After all, much gets thrown out with stale bakery products, for instance, or flat soda or the juice at the bottom of a cup or can. The authorities base these estimates primarily on surveys in which individuals are asked to recall what they ate and drank. This survey data is known to be exceedingly unreliable, which the USDA readily admits. (Limitations on accurately measuring food loss,
it says, suggest that actual loss rates may differ from the assumptions used.
)
Still, the USDA now reports that in 2014 (the latest numbers available as I write this) the average American consumed only 67 pounds of the sucrose and HFCS out of the 114 pounds the industry made available — slightly less than 60 percent. By doing so, a reasonably reliable number (114 pounds delivered) has been transformed into an unreliable number (67 pounds consumed). A number that can be used for historical trends and comparisons has been converted into a number that cannot.
The sugar industry prefers the latter, smaller number — We perceive it to be in our interest to see as low a per-capita sweetener consumption estimate as possible,
as one sugar industry executive wrote in a 2011 e-mail. The smaller number suggests that we don't eat or drink all that much sugar (or HFCS), after all. But it has no comparison. We have no meaningful way of adjusting sugar deliveries for loss decades or centuries ago. Nor can we use it to draw meaningful comparisons to the amount of other foods we supposedly consume today, because those adjusted numbers are also based on unreliable surveys and unsubstantiated assumptions.
For the sake of simplicity, I will typically refer in the text to the amount of sugar consumed per year (100 pounds per capita in the U.S. in 1920, for instance) because that’s how it was referred to in the documents I cite, even though this number was technically the amount of sugar made available by industry, i.e., deliveries. When I refer to numbers that purport to be legitimate estimates of consumption, I will be explicit. It’s a confusing business, but I’ll do my best to keep it clear as we continue.